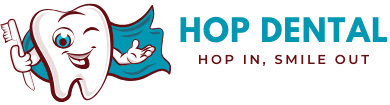
Tooth Abscess Stages: Early Signs to Dangerous Complications
Ignoring a tooth abscess can be terrifying, the stages move quickly from mild swelling to dangerous infection.
But don’t panic, in this guide on tooth abscess stages, we’ll show you exactly what to expect and how to take action before it’s too late.
The 5 Tooth Abscess Stages:
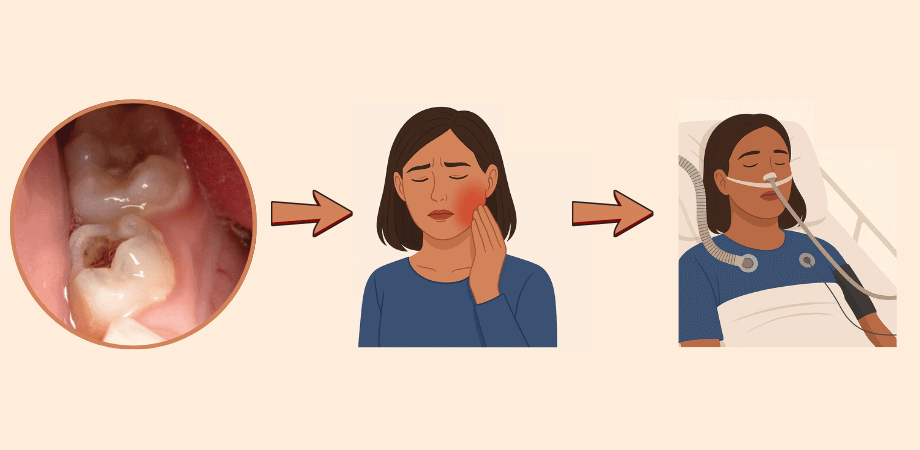
Stage 1: Early infection – The First Warning Signs
Early infection or pulpitis, is the very first stage of a potential tooth abscess. It occurs when bacteria start to penetrate the enamel, the hard protective layer of your tooth and reach the dentin underneath. This irritates the pulp, the inner part of the tooth containing nerves and blood vessels.
At this stage, the infection is just beginning, so acting quickly can prevent it from turning into the second stage “the irreversible pulpitis”.
Symptoms
Even though pain may be minor, this stage is critical because it’s your chance to stop the infection before it worsens.
Treatment
Immediate Relief: These are steps to reduce discomfort while waiting to see your dentist:
- Take over-the-counter pain relievers like acetaminophen if safe for you.
- Avoid chewing on the affected tooth.
- Rinse your mouth with warm salt water to reduce bacterial buildup and soothe irritation.
- Maintain excellent oral hygiene: brush gently with fluoride toothpaste and floss carefully.
Definitive Treatment: This is the treatment that addresses the early infection fully:
- Dental filling: If decay is caught early, the dentist removes the decayed area and fills it by composite (white fillings) or amalgam (silver fillings).
- Pulp protection: Sometimes a medicated liner is applied to protect the pulp.
- Root canal: In rare cases at this stage, if pulp inflammation is severe, a minor procedure may be required to prevent progression.
FAQ About The Early Stage of Tooth abscess
| 💬 Can this early infection go away on its own ? |
| ✅ No. The infection won’t disappear by itself, ignoring it allows bacteria to reach the pulp and form a full abscess. |
| 💬 How soon should I see a dentist? |
| ✅ Ideally within a few days. The earlier you act, the less invasive and painful the treatment will be. |
| 💬 Can I use home remedies to stop it? |
| ✅ Rinses like warm salt water can help with mild discomfort, but they cannot stop the decay or infection from progressing. |
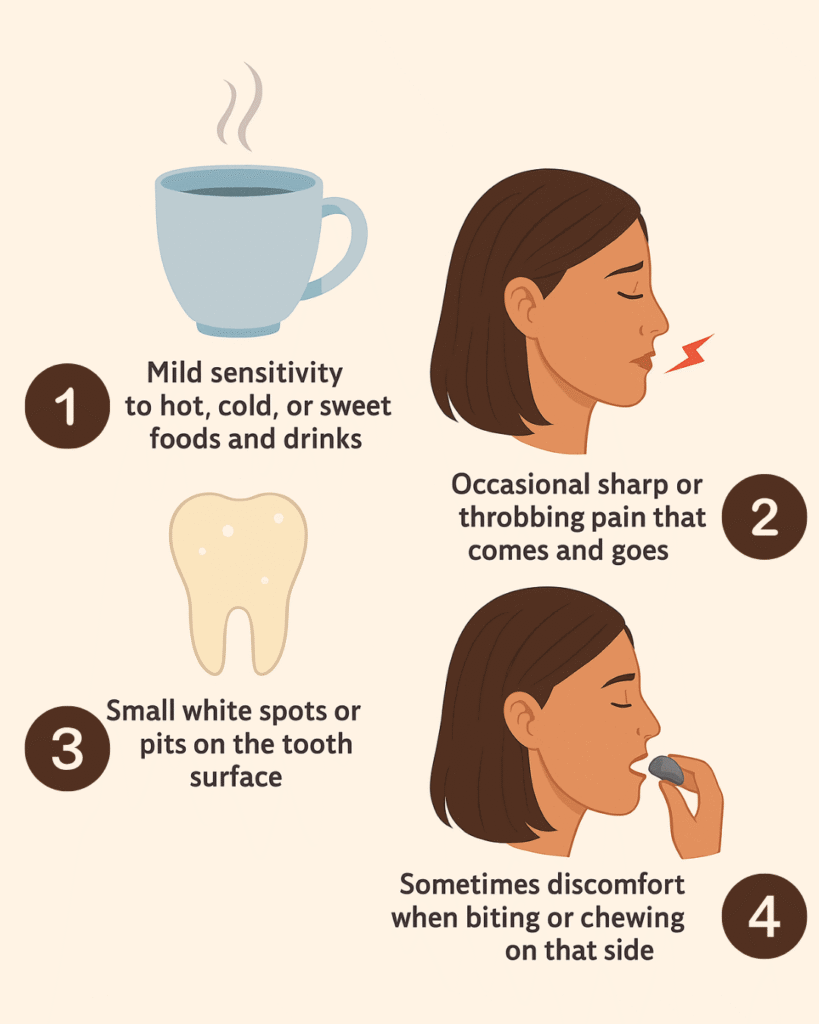
Stage 2: Infection spread to the pulp (irreversible pulpitis)
At this stage, the infection has fully reached the tooth’s pulp, the nerves and blood vessels inside the tooth. This condition is called irreversible pulpitis, meaning the pulp is inflamed beyond repair. The tooth can no longer heal itself, and without treatment, the infection may progress to a full dental abscess.
Symptoms
- Sharp, constant tooth pain that can radiate to the jaw, ear, or head.
- Pain intensifies with hot or cold foods and sometimes even without stimuli.
- Swelling of the gum near the affected tooth may begin.
- Sensitivity to biting or pressure.
- Occasionally, the tooth may feel loose or higher than the surrounding teeth.
This stage is usually much more painful than early pulpitis and signals the need for immediate dental care.
Treatment
Immediate Relief: At this point, the pain can feel unbearable. The only real way to calm it down before your dental appointment is by taking anti-inflammatory medications like ibuprofen.
But here’s the catch: while these drugs ease the pain, they also suppress your body’s natural inflammation. That means the infection can silently advance, moving faster from pulp inflammation to a full-blown abscess. Unless an antibiotic is prescribed to control the bacteria, the infection is free to spread.
Bottom line? Anti-inflammatories may buy you a little time, but they don’t fix the problem. The real relief only comes when your dentist removes the source of infection through a root canal or, in some cases, extraction.
Definitive Treatment: Since the pulp is irreversibly damaged, treatment focuses on removing the infection and saving the tooth if possible:
- Root canal therapy: The dentist removes infected pulp, sterilizes the canals, and fills them to prevent further infection.
- Dental crown: Often placed after a root canal to restore the tooth’s strength and function.
- Extraction: If the tooth is too damaged or the infection is severe, removal may be necessary.
Note: Antibiotics may be prescribed only if the infection is spreading or swelling is significant, but they are not a substitute for dental treatment.
Irreversible Pulpitis FAQ
| 💬 Can I wait a few weeks to see the dentist? |
| ✅ Waiting can be dangerous. Pain may worsen, and the infection can spread to surrounding tissues, leading to an abscess or more serious complications. |
| 💬 What if I can’t afford a root canal? |
| ✅ In some cases, extraction is a simpler and more affordable solution, but it’s best to discuss options with your dentist to prevent the infection from spreading. |
Stage 3: Abscess formation (localized pus pocket)
At this stage, the infection has progressed beyond the pulp and has formed a localized pus pocket, usually at the tip of the tooth’s root. This is a true dental abscess. The body is trying to contain the infection, but if left untreated, the abscess can grow, destroy surrounding bone, and spread to nearby tissues.
Symptoms
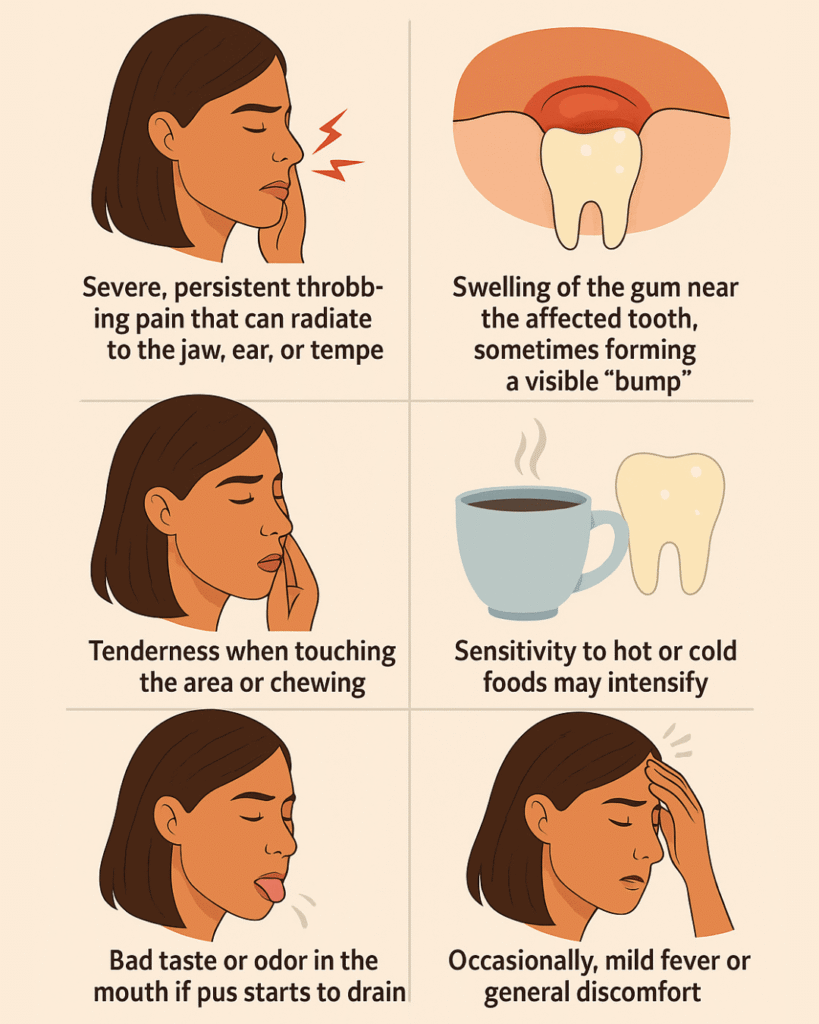
At this stage, pain is usually more noticeable and alarming, prompting most patients to finally seek treatment.
Treatment
Immediate Relief:
- Take over-the-counter pain relievers like ibuprofen or acetaminophen for temporary comfort. However, keep in mind that painkillers only mask the symptoms but they don’t stop the infection. In fact, suppressing the inflammation without treatment can allow the abscess to spread quickly and even turn into cellulitis. That’s why it’s critical to see a dentist as soon as possible.
- Apply a cold compress externally to reduce swelling.
- Avoid chewing on the affected side.
- Rinse with warm salt water to keep the area clean.
Definitive Treatment:
- Abscess draining: The dentist or endodontist will make a small incision to drain the pus and relieve pressure.
- Root canal therapy: If the tooth can be saved, the dentist removes infected pulp, cleans and fills the canals.
- Extraction: If the tooth is too damaged or the infection severe, removing the tooth may be necessary.
- Antibiotics: Prescribed if the infection is spreading beyond the localized area, but not a substitute for dental treatment.
Note: Treating the abscess promptly prevents serious complications, including spread to jawbone or bloodstream.
FAQ About Abscess Formation: What Patients Usually Worry About
| 💬 Can an abscess go away without draining? |
| ✅ No. The abscess will not heal on its own. Without treatment, it can worsen and spread the infection. |
| 💬 Is it safe to take antibiotics only? |
| ✅ Antibiotics may control infection temporarily but won’t remove the pus or fix the tooth. Dental treatment is required. |
| 💬 What if I can’t afford immediate treatment? |
| ✅ Seek emergency dental clinics or community health services. Ignoring an abscess can lead to severe complications. |
| 💬 How fast can an abscess worsen? |
| ✅ It can worsen within days, causing severe pain, swelling, and even systemic infection if left untreated. |
Stage 4: When The Infection Spreads Beyond The Tooth
At this stage, the infection has spread beyond the tooth and localized abscess, reaching surrounding tissues such as the gums, jawbone, or facial soft tissues. This is called cellulitis and can lead to serious complications if not treated immediately. The tooth’s surrounding bone may also begin to erode.
Symptoms
- Severe, persistent pain that worsens with time.
- Swelling of the face, jaw, or gums near the infected tooth.
- Redness and warmth in the affected area.
- Fever, fatigue, or general malaise.
- Difficulty opening the mouth (trismus) or swallowing.
- Sometimes the tooth may feel loose or elevated.
At this point, the infection is no longer localized, and urgent professional care is required.
Treatment
Immediate Relief: At this stage, over-the-counter painkillers are no longer enough. The infection is spreading beyond the tooth and can quickly become life-threatening.
The only immediate step is to seek urgent dental or hospital care. Temporary comfort may come from cold compresses and keeping the head elevated, but antibiotics and professional drainage are absolutely required
Definitive Treatment:
- Hospital or emergency dental care: Cellulitis and bone involvement can be serious; immediate evaluation is necessary.
- Antibiotics: Strong prescription antibiotics are often required to control the infection.
- Drainage: If the infection forms pockets or spreads into soft tissues, surgical drainage may be needed.
- Tooth extraction or root canal: The damaged tooth may need extraction, or if possible, a root canal may save it.
- Bone treatment: If bone is affected, further procedures like debridement may be necessary.
Note: Delaying treatment can result in life-threatening complications, so this stage is considered a dental emergency.
What to know about the fourth stage: FAQ Answered
| 💬 Can cellulitis from a tooth infection be life-threatening? |
| ✅ Yes. If the infection spreads to deep facial spaces or bloodstream, it can be very dangerous and requires urgent care. |
| 💬 Are antibiotics alone enough? |
| ✅ No. Antibiotics can control the spread temporarily, but the source of infection must be treated by a dentist or surgeon. |
| 💬 Can I go to a regular dentist at this stage? |
| ✅ If swelling is severe or affecting breathing or swallowing, go to the emergency room. Otherwise, contact a dentist immediately for urgent care. |
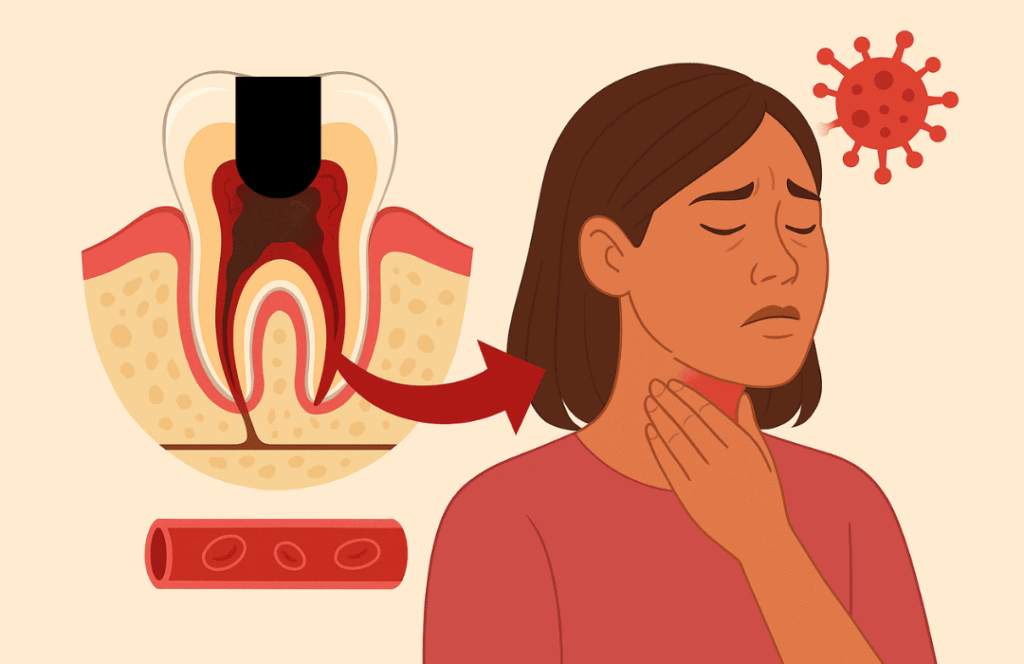
Stage 5: Systemic complications (sepsis, serious risks)
This is the most severe stage of a tooth abscess. The infection has spread from the tooth and surrounding tissues into the bloodstream or other parts of the body, causing a life-threatening condition called sepsis. At this stage, the infection can affect multiple organs and become fatal if not treated immediately.
Symptoms
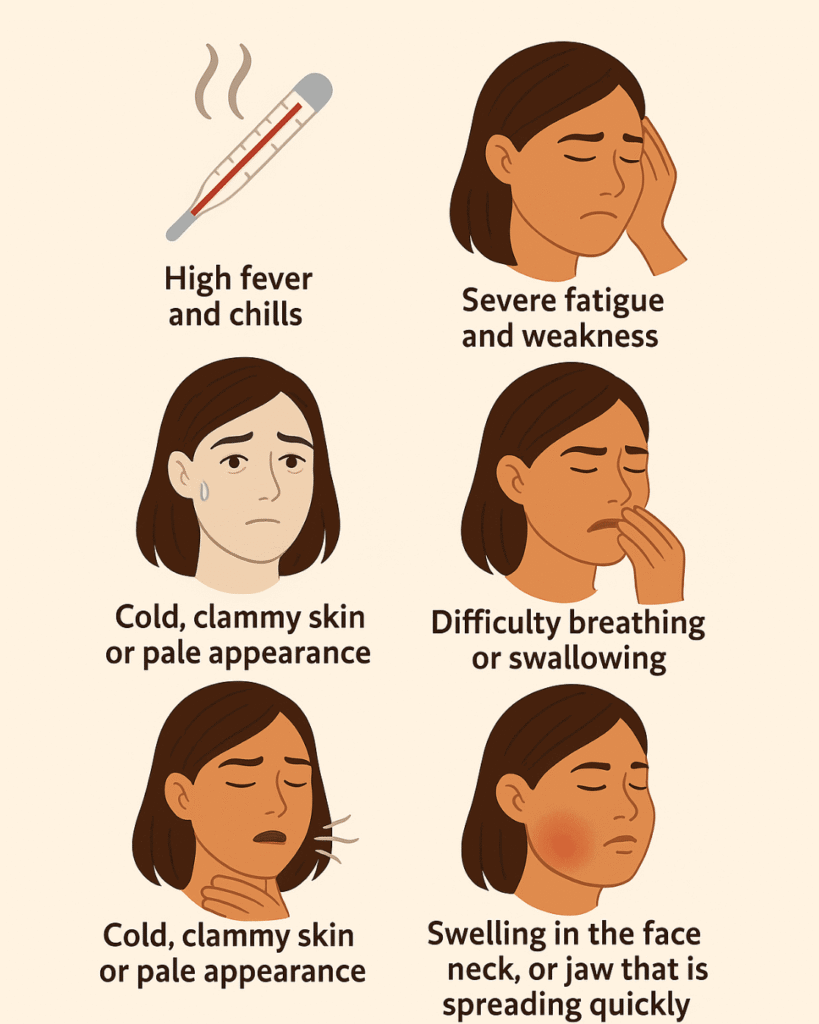
This stage represents a medical emergency, and immediate attention is required.
Treatment
Immediate Relief: At this stage, home remedies are no longer effective, Call 911 or go to the nearest emergency room immediately. This stage is life-threatening.
Keep the patient calm and in a semi-upright position if swollen areas affect breathing.
Definitive Treatment:
- Hospitalization is usually required.
- Intravenous (IV) antibiotics to control the infection quickly.
- Surgical drainage of any remaining abscesses in the mouth or jaw.
- Removal of the infected tooth to eliminate the source of infection.
- Supportive care for organs affected by sepsis (fluids, monitoring, intensive care if necessary).
Here’s a quick breakdown of the five stages of a tooth abscess, including the key symptoms to watch for and when the situation becomes truly dangerous.
| Stage | Main Symptoms | When It Becomes Dangerous |
| 1. Early Infection | Mild sensitivity, gum redness, slight discomfort | If ignored, cavity or gum irritation worsens |
| 2. Pulp Inflammation | Sharp pain, especially at night, sensitivity to hot/cold | Infection can reach the root and form abscess |
| 3. Abscess Formation | Throbbing pain, visible swelling, pus pocket | Infection spreads to jaw or surrounding tissues |
| 4. Severe Abscess | Intense pain, fever, facial swelling, difficulty eating | Risk of sepsis and spread to bloodstream |
| 5. Systemic Complication | High fever, weakness, fatigue, breathing issues | Life-threatening, emergency care required |
Tooth Abscess Stages FAQs: Real Questions Patients Ask
What are the first signs of sepsis from a tooth abscess?
The first signs of sepsis from a tooth abscess can feel like your body is fighting more than just a toothache. Early red flags include:
- Fever and chills that come on suddenly
- Rapid heartbeat or breathing
- Extreme fatigue or weakness
- Confusion or feeling “out of it”
- Sweaty, clammy skin
These symptoms mean the infection is moving beyond the tooth and spreading into the bloodstream a dangerous stage that requires emergency care.
Dentists often describe the tooth abscess stages to explain how a simple dental infection can escalate: what begins as localized pain and swelling can, if ignored, turn into a life-threatening systemic infection.
If you ever notice these warning signs along with a dental abscess, call emergency services right away. With sepsis, every hour counts.
how long until a tooth infection kills you?
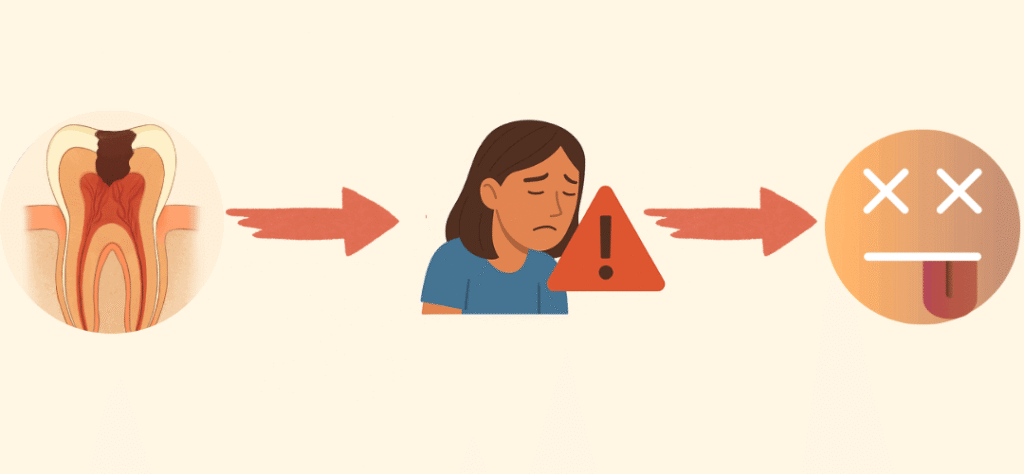
A tooth infection won’t kill you overnight, but ignoring it can be extremely dangerous.
Dental abscesses usually progress in stages what dentists call the tooth abscess stages. At first, it may just feel like sensitivity or swelling around the gum. If left untreated, the infection can spread deeper into the jaw, then into the bloodstream, leading to a life-threatening condition called sepsis.
For most people, this doesn’t happen immediately; it can take days to weeks, depending on your overall health and how strong your immune system is.
But here’s the key: once the infection spreads beyond the tooth, things can escalate very fast. That’s why any sign of a dental abscess severe toothache, swelling, pus, or fever should be treated as an emergency.
The bottom line? Don’t wait and wonder “how long until a tooth infection kills you.” See a dentist right away. Early treatment is simple and safe. Waiting can be dangerous.
How do I know if a tooth infection has spread to my brain?
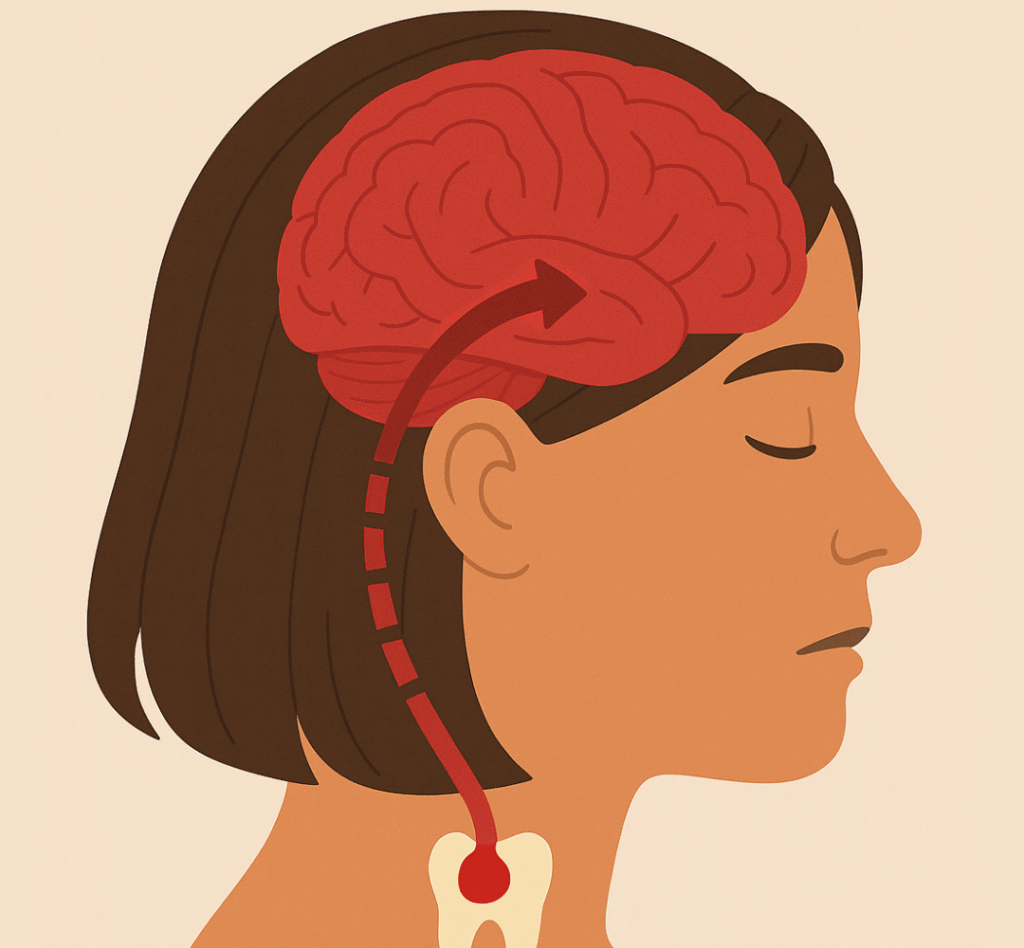
A tooth infection spreading to the brain is rare, but it can happen if a dental abscess is left untreated. The warning signs go beyond typical toothache. If the infection has started spreading, you may notice:
- Severe, throbbing headache that doesn’t go away
- Swelling around the eyes or face
- Vision changes or confusion
- Fever, nausea, or vomiting
- Seizures or difficulty moving/talking in extreme cases
These are red flags that the infection is no longer just in your tooth. In fact, dentists describe the tooth abscess stages to show how an infection can progress from a simple pocket of pus in the gum to a dangerous, whole-body threat.
Understanding the phases of a tooth abscess can truly save not just your smile, but sometimes your life. From the first signs of pulp inflammation to the dangerous progression that can trigger sepsis, every stage carries warning signals you shouldn’t ignore. Acting early and getting timely dental care makes all the difference.
The good news? Most dental abscesses are treatable, and with good oral hygiene and regular check-ups, you can stop them from ever progressing to advanced stages. Your teeth and your overall health are worth the attention, so don’t wait until pain or swelling takes control.
Let’s Hear From You!
Have you ever dealt with a dental abscess or noticed the warning signs early? Share your experience or questions in the comments, your story might be the push someone needs to seek help in time.